Post surgical care
Following your procedure a dressing will be placed over the wound. In most cases this should be kept dry for at least the first 24 hours. It can then be removed and gently washed with soapy water. If there are strips of tape over the wound these should be left in place until they fall off. The wound should then be patted dry and a new non-stick dressing placed over the wound. This can be repeated once to twice daily after a bath or shower. If the dressing becomes wet it is important to change the dressing.
Wounds heal much better in a closed environment so it is important to keep the wound dressed until the sutures are removed.
It is expected that you may have some discomfort after the procedure. Regular paracetamol and if possible raising the affected part of the body should be sufficient to manage the pain. If it is throbbing and the pain increasing it may indicate a need to see your doctor. You should also keep an eye out for other signs of infection including redness, heat and discharging pus.
After the local anaesthetic wears off there may occasionally be some more bleeding. Leave the dressing in place and apply direct pressure over the top for 15 minutes. This will usually stop most bleeding, if it does not you should see your doctor. If the dressing becomes soaked then it should also be changed.
The sutures and subsequent scar are not as strong as your normal skin. Especially in the first few days but even for a few weeks you should be mindful of your activities and attempt not to pull the wound apart with your movements.
At the time of the procedure your doctor will book you an appointment for the removal of your sutures. They will discuss the results of the pathology at the time also. However if you have any concerns about your wound then please present earlier.
Scar management
Scars are an inevitable part of undergoing an excision and unfortunately impossible to avoid. At all times we attempt to minimize the scarring and aim for a fine white line. This is not always possible and many factors influence scarring and so can be out of our doctors control. Some of the factors include the size of the wound and defect, the resulting tension on the wound, infection, the location on the body (some parts heal better then others), genetic factors that is, some people are prone to large scars and the post operative care and types of dressings used.
There are some steps you can take to help to minimise the scarring after your procedure. It is important to keep your wound covered until it is healed, i.e the sutures removed. Wounds heal much better in a closed environment. Silicone gel has been proven to be quite effective at reducing scarring. After the sutures are removed apply the gel once daily over the scar. This should continue for 3-6 months for the best results. A commercially available gel called Strataderm can be bought from most pharmacies. Taping the scar has also been an effective way to reduce the scar.
The risks of surgery include Keloid and hypertrophic scars. This occurs when the body forgets to flip the switch to stop the healing and scar tissue continues to be laid down. It results in a raised thick scar that can be itchy or even painful. Some people are more prone to these and they tend to occur more commonly on the chest and backs. Silicone gel works well to reduce the scar. In more severe cases hydrocortisone injection into the scar can be performed. Very occasionally the scar can be excised but this of course runs the risk of creating a new scar in its place.
Prevention
Overwhelming scientific evidence confirms that a majority of skin cancers are as a result of exposure to UV radiation from the sun. Many of these skin cancers are entirely preventable by taking precautions to shield yourself from the sun’s rays. Guidelines currently recommend that precautions be taken for any exposure when the UV index is above 3. In Townsville in summer the UV index will be above 3 from about 7:30am to about 5:30pm whilst in winter it is more like 9:30am to 2:30pm. Many weather phone apps or websites can give you the current UV reading.
If possible try and plan your day to avoid being outside during very high UV periods, otherwise utilize shady areas. Remember even on overcast days the UV rays will still penetrate cloud layers and be potentially damaging to your skin.
During the times of higher UV readings the best course of action is to cover up as best as you can. Wear a long sleeved shirt with collar and buttons done up, long pants, a broad brimmed hat and wrap around sunglasses.The eyes are not immune to cancers from UV exposure.
Sunscreen has been proven to prevent all sorts of skin cancers and it should be used on the parts of the skin that are exposed. Sunscreen will wear off and it should be reapplied liberally every 2 hours.
It is easy to get caught out and that is why covering up is better. When looking for a sunscreen it should be at least 30+ and broadspectrum, that is it has protection against UVA and UVB radiation. Many moisturiser and make up products contain sunscreen which is great. But just remember their effectiveness will diminish throughout the day and require reapplication.
Sunscreens
UV radiation from the sun contributes to the formation of many skin cancers and it is widely acknowledged that sun protection is important to prevent their formation. Sunscreen is an important part of sun safe behaviour and has been proven to prevent basal cell carcinoma (BCC), squamous cell carcinoma (SCC), melanoma as well as prevent ageing as a result of sun exposure.
Ultraviolet radiation is produced by the sun and is divided into 3 categories according to wavelength.
UVA - 320-400nm
UVB - 290-320nm
UVC - 260-290nm
UVC radiation is mostly absorbed by the earth’s atmosphere. UVB is responsible for sunburn and DNA damage in skin cells resulting in BCCs, SCCs but also melanoma. UVA penetrates deeper in the skin and exposure causes tanning. It has been implicated in contributing to the development of melanoma as well as aging of skin. The concentration of UV radiation is higher with closer proximity to the equator, at higher altitudes and in summer. Whilst UV levels are higher on a clear cloudless day up to 85% of UV rays will penetrate the clouds, so sun protection is still crucial on overcast days.
Self checks
Whilst many skin cancers are slow growing, subtle and insidious others can appear and grow rapidly and be more aggressive. It is important to get to know your own skin to help to identify any potentially dangerous skin lesions between your regular skin checks with your doctor.
Skin checks should occur regularly enough that they become a habit without becoming bothersome, every 1-2 months is a good time frame. Your entire body should be examined including the soles of your feet and scalp. You may need to use a mirror or have someone else to help with the parts you cannot see. Sometimes it is good to keep a body map where you can mark suspicious lesions or take photos of body parts that you can refer back to as a reference point.
What do I look for?
A simple acronym of SCAN will help you to identify suspicious lesions
S - SORE
Scaly, sore, tender, itchy or hasn’t healed in 6 weeks
C - CHANGING
Changing is size, shape colour or texture
A - ABNORMAL
Looks or feels different or stands out when compared to other moles or spots on your body
N - NEW
Has appeared on your skin recently. Any new moles or spots should be checked, especially if you are over 40.
Melanomas especially can look like anything so it can be difficult to tell you exactly what to look for. If anything stands out and doesn’t look like anything else on your body it is best to have it looked at by your doctor. It can be very difficult with the naked eye but with the aid of a dermatoscope your doctor can diagnose with a lot more confidence
Am I at risk?
Skin cancers can arise in anyone however some will be at a higher risk of developing skin cancer than others. Some risk factors include
Fairer skin that does not tan and easily burns
Increased number of moles
A family history of skin cancer or melanoma
Amount of sun exposure especially in childhood
Increased age
Being male
You can gauge your risk by completing the following questionnaire or visiting http://www.scanyourskin.org/risk-prediction-tool/
1. What is your gender?
Male (1) Female (0)
2. What is your age group?
60+ (2) 40-59 (1) 39 or less (0)
3. What is your ethnic origin based on the majority of your ancestors?
Northern Europe, Ireland or UK (1) Other (0)
4. When you went out in the sun without sunscreen, did you burn easily and never tan, (or only tan a little bit)?
Yes (1) No, I could get a tan (0)
5. Since you were born, how many times have you been so severely sunburnt that your skin peeled and blistered?
More than 5 (2) 2 to 5 (1) Less than 2 (0)
6. As a teenager, how many moles and/or freckles did you have?
Many (2) Some (1) Few or none (0)
7. Has anyone in your immediate family had a melanoma? (This is the most dangerous type of skin cancer and is always treated by surgical removal)
Yes (1) No (0)
8. Have you had any sunspots burnt or frozen off?
More than 10 (3) 1 to 10 (2) None (0)
9. Have you had any type of skin cancer cut out? (e.g. BCC, SCC, Melanoma)
More than 10 (6) 1 to 10 (4) None (0)
10. Were any of the skin cancers in question 9 a Melanoma?
Yes (3) No (0) Not applicable (0)
Add the scores of your responses and determine your risk
Score: 9 + Risk: High
What you should do…
See a doctor for a full-body skin check as soon as possible.
SCAN your skin yourself every 3 months.
Have a full-body skin check at least once a year.
Score: 4 to 8 Risk: Medium
What you should do…
See a doctor for a full-body skin check.
SCAN your skin yourself at least twice a year.
Have a full-body skin check every 2-3 years.
Score: 0 to 3 Risk: Low
What you should do…
See a doctor for a one-off skin check, or if you have any concerns.
SCAN your skin yourself at least once a year.
Remember – Low risk doesn’t mean NO risk.
Note: The information provided by this tool is to be used as a general guide and not to be solely relied upon. It is highly recommended that you discuss your personal risk factors and results of this risk assessment with your doctor.
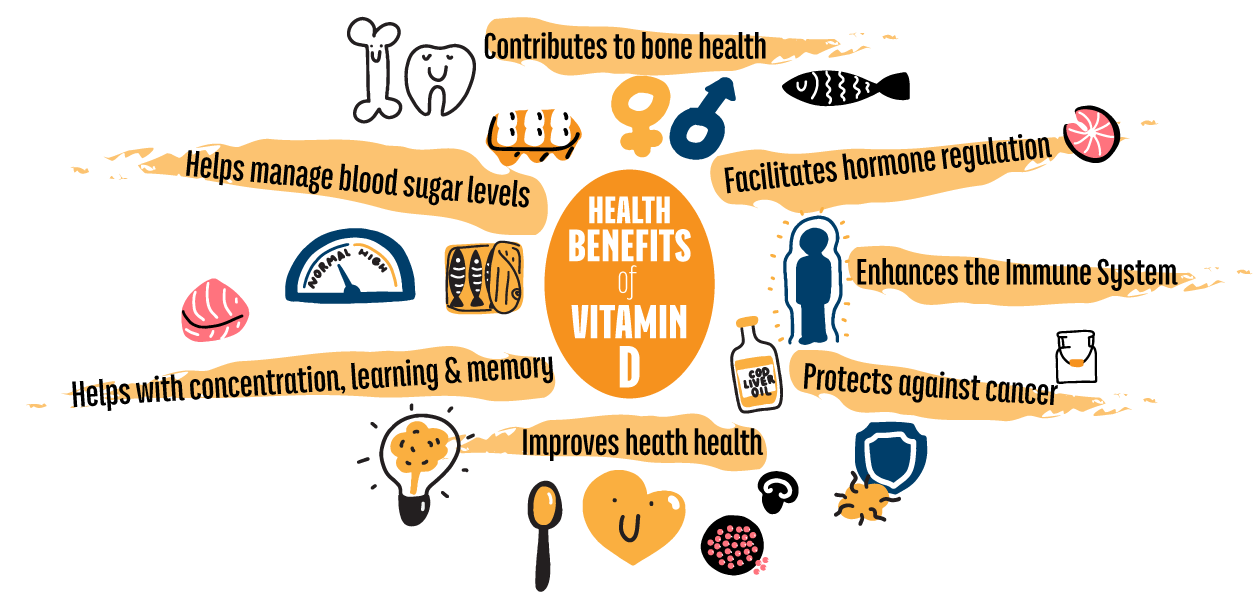
Vitamin D
Vitamin D is a hormone that controls calcium levels in the body. Adequate levels are important to maintain healthy bones and muscles. A small amount of vitamin D is derived from the foods we eat, mainly fish and eggs. However the vast majority of vitamin D is synthesized in our skin through exposure to UV radiation from the sun.
Our skin is very efficient at this production and it occurs very quickly. It is important to note that vitamin D is not ‘stockpiled’ and only a certain amount can be produced and stored in a single day. On a typical North Queensland day vitamin D production will max out within 5 minutes of sun exposure, if your skin has turned red then you have well and truly finished vitamin D production and now only sustaining damage from the sun. The UV index will vary throughout the year but remains above 3 for the vast majority of time in North Queensland. At this level it has been shown that a few minutes a day whilst wearing a shirt, hat and sunscreen is enough to maintain adequate levels of vitamin D. For most people this occurs whilst going about your daily activities.
Vitamin D deficiency is more likely to occur in certain populations and situations. People with very limited sun exposure may be at risk. This includes those wearing clothing to cover their entire body for religious reasons, those who remain nearly completely indoors for example institutionalised and those in locations with limited hours of sun, ie Tasmania or the UK, especially in winter. North Queensland has around 264 days a year of sun so this is generally not an issue here.
Melanin the pigment in skin protects our cells from damage from UV radiation, it can also make vitamin D production more difficult. So dark skin individuals may be susceptible to deficiency. This is more likely to be in places with limited sun however. Other special groups include exclusively breastfed infants, so breastfeeding mothers may need to have supplemental vitamin D. The elderly as vitamin D production becomes less effective with age. Those with fat absorption defects including those who have had gastric bypass surgery and obesity.
Vitamin D deficiency can result in osteoporosis where bones become weak and prone to fractures. In children it will cause Rickets characterized by soft and weak bones and stunted growth. Vitamin D deficiency has been thought to be associated with increased cancer risk. There have been many studies performed with a great deal of variability. Some found vitamin D supplementation reduced cancer risk, some found no change at all whilst others found it actually increased risk. As such no clear consensus has been reached. What is very clear is that excess UV radiation is responsible for a vast majority of skin cancers, so the risks of excess UV exposure from the sun outweigh the benefits.
Queensland has the lowest rates of vitamin D deficiency in Australia with 94% of people with adequate levels in summer and 85% in winter. If there are concerns about your vitamin D levels they can be checked with a blood test. If they are low they can be supplemented with a safe and well tolerated medication. Whilst it is true sunscreen can impair vitamin D production, studies have shown that its use does not result in vitamin D deficiency.