Skin Checks
Some skin cancers are obvious and many people will identify them themselves. Others are more subtle and difficult to recognise with the naked eye. Skin cancers are more common in sun exposed areas but they can occur anywhere including parts of the body that do not see the sun. It is important to see a doctor from time to time for a full body skin check. Different people are at different risks so the frequency of these checks may vary for everyone. Your doctor will guide you on a good time frame.
Skin checks are generally considered screening, that is the aim is to identify something you were not aware of. Sometimes if you present with a suspicious lesion the doctor may opt to do a full skin check as well. As skin cancers can occur anywhere a skin check is best performed in your underwear. You can cover with a sheet if you feel more comfortable. The doctor will examine your skin from head to toe with the aid of a dermatoscope. This is a special device that uses polarized light and magnification to see into the skin and make diagnosis easier.
Occasionally the doctor may take photos of suspicious lesions. They can then enlarge them on a computer screen. They may decide to review the lesion in a few months or if it is more suspicious have the lesion biopsied or even excised. This generally occurs on another day.
We do ask when you come for a skin check to please refrain from wearing makeup, creams or moisturisers as this can make it more difficult to properly view your skin. But of course deodorant is fine. Occasionally skin cancers can grow beneath your finger and toenails so it is best to have any nail polish removed also.
Whilst it can be a little daunting having your skin examined for some people we do try to make you as comfortable as possible and a positive experience.
Total Body Photography
People with a very large number of moles on their skin, particularly those that vary in size and shape are at a higher risk of melanoma. Generally melanomas are new lesions that exhibit change over time. The difficulty can be ‘picking the needle in the haystack’ as the melanoma may blend with the other moles.
Some high risk patients may benefit from total body photography. This involves taking several photographic images of different body parts to build a representation of the full body. These can be used as reference points to detect any change for the patient when doing self checks at home or for the doctor whilst performing routine skin checks.
It is best if the photographs are updated every few years.
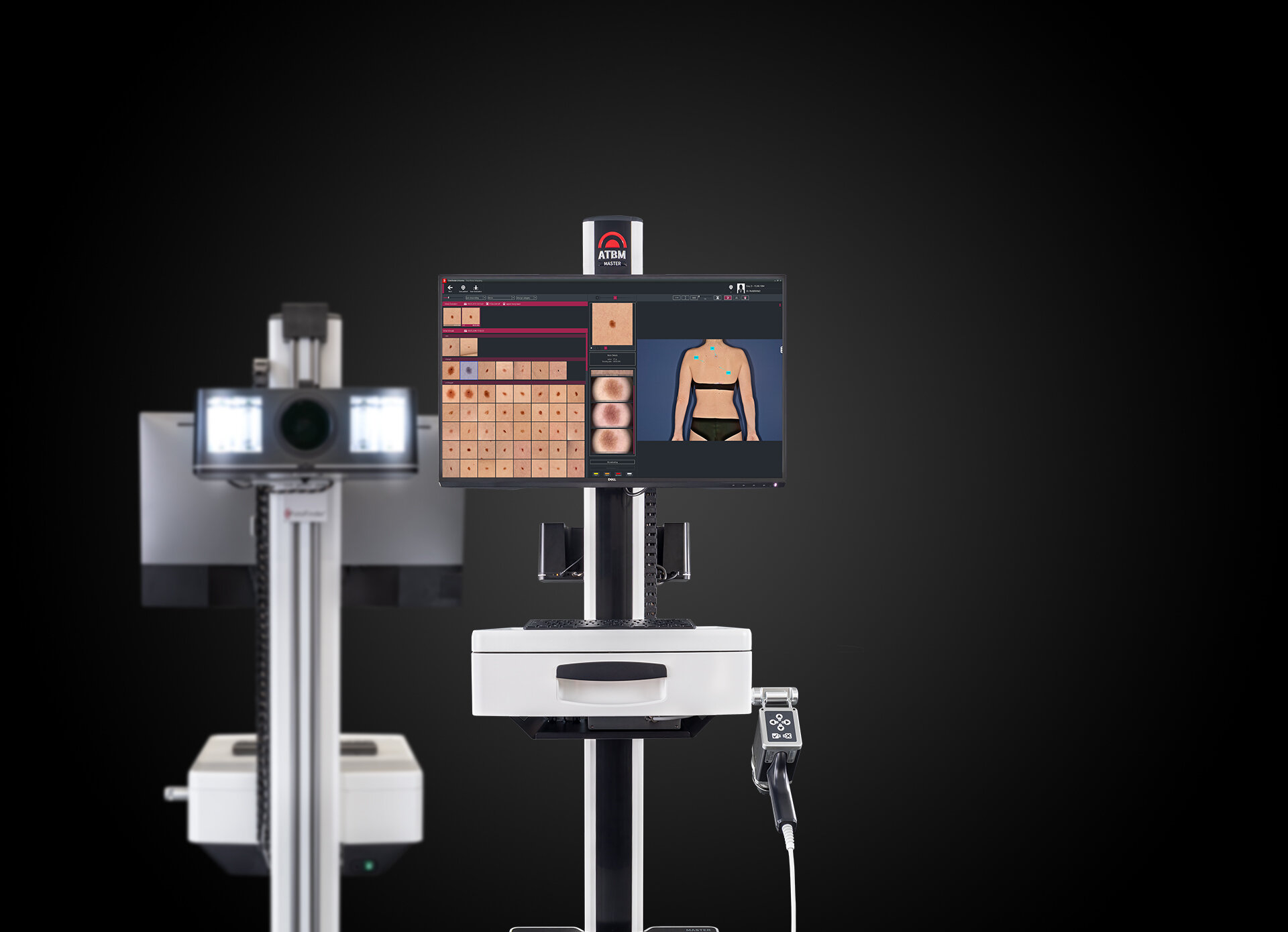
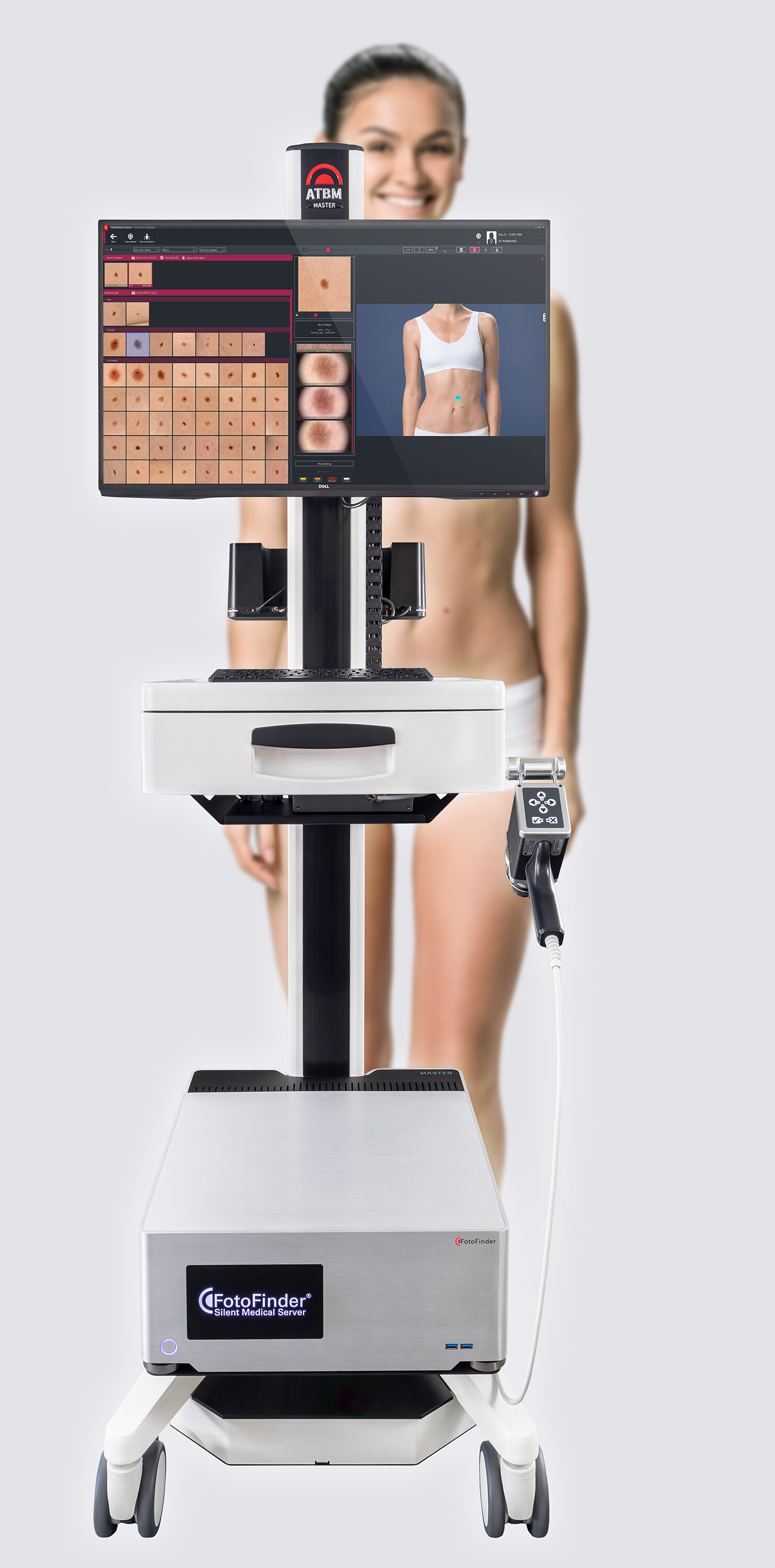
Fotofinder Automated Total Body Photography
Early detection of melanoma is the key to improving prognosis. We know that 70% of melanomas are new lesions not arising from an existing mole whilst other melanomas will exhibit change over time. Identifying these new and changing lesions in high risk patients that have a very large population of moles can be difficult. Total body photography and body mapping has been used to help detect these changes.
North Queensland Skin Centre utilises the Fotofinder Automated Total Body Mapping (ATBM) System to aid in detecting new and changing lesions. It creates an accurate skin map of a patient in less than five minutes. The Fotofinder ATBM posesses an ultrahigh definition 50mp automatic camera with a polarized lens for the clearest and defined images. The camera is mounted on a computer controlled lift mechanism and moves to exact levels to take four photos of each side of a patient in quick sequence. These photos are stitched together to eliminate overlapping redundant areas and create an accurate skin map. This set of high-resolution photos are used as reference for follow up skin exams and allows the detection of new and changed moles.
The initial scan simply acts as a baseline, the software will not detect suspicious lesions on this scan. It is on follow up scans that the benefits are really realized. By comparing baseline and follow up mole mapping photos, the Fotofinder ATBM can automatically identify new lesions and visible changes in existing moles and assist the doctor in the detection of skin cancer.
The on-screen comparison of total body photography images is significantly easier and faster then traditional mole mapping methods. This is in part due to the consistency of patient position and lighting as well as improved image definition and analytical software. This increased accuracy enabled the Fotofinder system to lay claim to identifying the smallest melanoma in the world at 0.9mm. Total body photography used to be a challenging and time consuming process. But with Fotofinder ATBM, full body photography can be done in less than five minutes
Automated total body mapping does not replace but rather is used in conjunction with a full body skin check by your doctor. By combining these two methods we are able to provide the gold standard in care for detection of melanoma and other skin cancers. Some private health insurance funds will also offer a rebate for the process.